[00:00:00] So the reason, that I’m able to help my clients get such great results is because I ask better questions. So instead of being limited to asking, what is the name of the disease and how are we going to treat it with medication or a prescription? I ask the question why. Why is this happening? Why is this person experiencing these symptoms?
[00:00:28] And then we have a whole lot more material to work with because we can get really specific in our questions that we’re asking.
[00:00:38] Hey, everyone. Welcome to The Nourished and Thriving Show. I’m your host, Katie Lovitt. I’m a registered dietitian on a mission to help you increase your impact and legacy on the world while healing your gut and reducing your IBS symptoms. I’m so grateful to have you here. Each week I’ll inspire you to live vibrantly and provide valuable resources and information that empowers you to take bold action towards your health goals. Before we dive in, make sure you follow or subscribe to my show wherever you’re listening so you never miss an episode. Ready? Let’s go!
The Question I’m Always Asked From Chronic Gut Symptom Sufferers
[00:01:17] Hey everybody. I’m so glad that you’re listening in today. So today we’re starting out with what may feel like a basic question… With a not so basic answer. So I’m really excited to dive into this. I wanted to start out with this, because it’s a question that I get asked a lot, not necessarily directly, but it’s the question that people are getting to.
[00:01:49] The question that I get asked a lot, or comments that are made are, “While I’ve tried things before or I’ve been to the doctor…” They basically threw their hands up in the air and said, “They didn’t know what to do to help.” So we’re gonna really unpack that because where does that leave people? If they feel like they’re, you know, not able to be helped, if there are no more answers for them and they’re really truly suffering and struggling to get by.
[00:02:16] That’s not a very great looking place to be, and that’s not a place I would wanna be. And it’s not a place that I want you to be either. So let’s start out by just unpacking a little bit more of this and why this is so important to me and why it’s important to you too. I know that most of you listening are probably really suffering from chronic digestive symptoms, whether it’s pain, bloating, urgency, constipation, heartburn, reflux, any of those things are lumped in I’m lumping into this category here.
How Your Digestive Problems are Typically Addressed by U.S. Doctors
[00:02:50] Right? So in fact you’re not alone and there’s actually about 74% of Americans living with these symptoms. Chronically that’s a lot of people, that’s a lot of Americans, right? That’s a lot, And so what happens whenever you’re doing this? So maybe you’re just surviving. Maybe you’re getting by day to day.
[00:03:17] Maybe it’s become your normal for you, but if you are at the point where you’re really needing help, which is oftentimes the case – this is actually a really big cost of medical care in the US is emergency room visits for chronic GI symptoms – that all of a sudden flares feel unbearable and people actually go to the emergency room.
[00:03:41] It’s a big reason for surgeries for major surgeries or these chronic GI symptoms. Say you get help and it’s not like an emergency room visit. You’re just like, I can’t deal with this anymore. Something’s going on. You go to your doctor, they inevitably will probably refer you over to a gastroenterologist / GI doc.
[00:04:01] And that GI doc is gonna do some screens. So whenever we’re looking at conventional medicine, they are looking to name what the problem is, what the disease is, because it’s pretty much gonna be a disease that they’re looking for. And then they’re gonna treat the disease. Okay. With medication surgery, some sort of intervention.
[00:04:22] So diagnose the disease and treat the disease, name it treatment. So you’re going in to try and find a name so that then you can find a treatment to your symptoms. Okay, so most of the time that looks like doing a colonoscopy and an endoscopy to see if there are signs of inflammatory bowel disease.
[00:04:44] So these are things like ulcerative colitis, Crohn’s disease, microscopic colitis. All of these more, you know, things that are visible on these scopes. Okay. And about 1.3% of Americans have inflammatory bowel disease. And in fact, this number is going up. We’re starting to see more and more kiddos presenting with inflammatory bowel disease.
[00:05:11] But if you have 74% of Americans struggling with chronic digestive symptoms and only 1.3% are getting diagnosed with this disease. What about everybody else? That’s still a lot of people, right? Over 72% of Americans are suffering without a name for their symptoms. So that’s when we’re gonna introduce IBS – irritable bowel syndrome.
[00:05:37] Now there’s a couple of different ways that we can look at IBS. There are some diagnostic criteria for it, and I’m gonna read these criteria out to you guys so that you know, what is recurrent, so that means happening over and over again. Abdominal pain that’s happening at least one day a week in the past three months with also at least two of these.
[00:06:09] So this pain is associated… This pain is happening when you’re going to the bathroom, having a bowel movement. Or you’re having pain with a change in the frequency of your bowel habits, or you’re having pain with a change in the form or appearance of your stool. Whenever you’re having a bowel movement, at least one day a week for at least three months with in the last three months with symptoms extending.
[00:06:39] Into the prior six months before that. So someone is experiencing these symptoms for six months, at least before they can even get this IBS diagnosis. Oftentimes IBS is also considered to be a diagnosis of exclusion. Now, what this means is just like I laid out before you go in, you have your colonoscopy, you have your endoscopy.
[00:07:03] Doc says, everything looks fine. I don’t know what’s wrong. You must have IBS. Okay. Let me know if that’s something that you’ve experienced before. Um, right. The doctors are in the name it and treat it business. That is what they have been trained to do is put a name on this thing. So we know what we’re dealing with.
[00:07:21] And then you know what protocol and treatment approach to do for it. The more accurately you can name something, the more accurate you can be of your treatment. Right? The problem is IBS is a really broad range of symptoms and there’s not a super specific definition for it. So about 15% of Americans are then diagnosed with IBS.
[00:07:47] So you have 15%, 1.3%. You have 74% of people having these symptoms. So what about everybody else? So that is why you’ll hear me talking a lot of the time about what I call the hot mess gut. Okay. A lot of people don’t have a disease diagnosis to go off of. There’s no treatment. And even people who do, if you have IBD, you know you’re most likely given some medication and just said, you know, “It’s something that you need to manage for the rest of your life, and take medication for the rest of your life.
[00:08:22] And hopefully it doesn’t get too much worse.” And with IBS, you’re probably told, “Try a low FODMAP diet, good luck. Here’s a pamphlet, which good luck with that because it’s a really confusing diet to follow.” Speaking from, you know, as a professional with experience in it, it’s tough. So if you’ve been able to follow it successfully on your own, like kudos to you, cause it’s –
[00:08:45] They may be able to give you some medication to help reduce your IBS symptoms. But other than that, they’re gonna throw their hands up and be like, “I don’t really know.” Now if you’re not even a person who’s been able to get a diagnosis, you’re probably being passed around from doctor to doctor, like, “Oh, we can’t find anything wrong with you.”
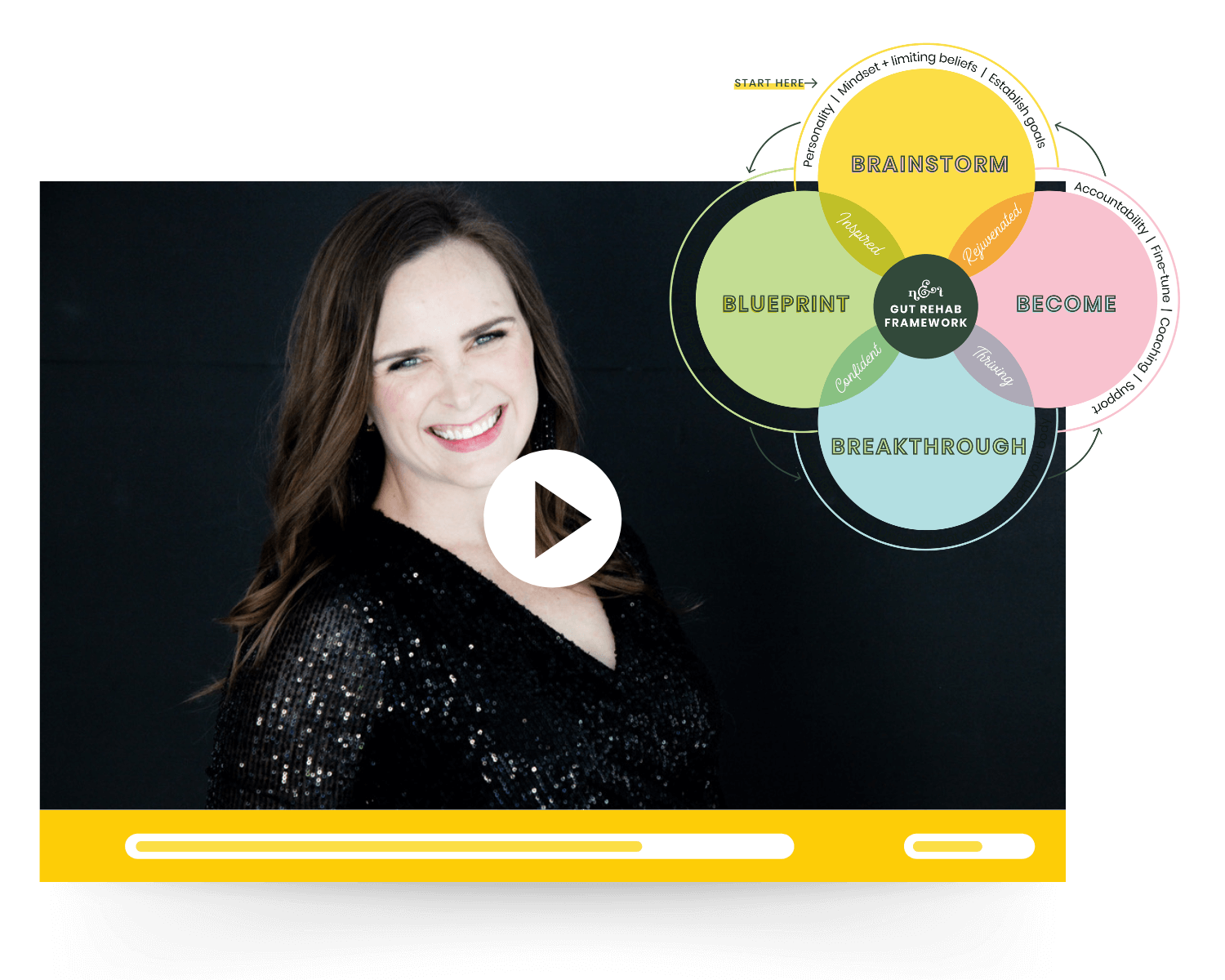
[00:09:02] “…Try this. Try this, try this, you know, go see this person, go see that person.” And you’re just going from person to person and reading books. Right? Then you start going into that root cause researcher mode, like we’ve talked about in our six stages of gut rehab, where you’re trying to find answers on your own because you haven’t really been able to get answers at the doctor’s office.
How I Typically Address Chronic GI Symptoms and Digestive Problems
[00:09:23] So the reason that I’m able to help my clients get such great results is because I ask better questions. So instead of being limited to asking, what is the name of the disease and how are we going to treat it with medication or a prescription? I ask the question why. Why is this happening? Why is this person experiencing these symptoms?
[00:09:51] And then we have a whole lot more material to work with because we can get really specific in our questions that we’re asking. And we can also get really broad and we can ask questions about triggers and patterns and, you know, ask really good questions. Spend a good chunk of time digging into this.
[00:10:17] Now, if you’ve gone to your doctor’s office, they’re seeing 30 to 40 patients a day, right? Their, their appointments are limited to 15 minutes. They don’t have the time or capacity to really dig into this with you. There are exceptions, but for the most part, our insurance model here in the U.S. is not supportive of doctors really being able to dig into the weeds with the patient.
[00:10:42] And that’s something that I am free to do in my approach. And most integrative and functional practitioners do as well. So we’re able to really ask good questions, piece things together. A lot of the time, honestly, people won’t send me information on their intake form whenever we’re starting out to work together.
[00:11:04] And then we have a conversation and I’m still asking even bigger, deeper questions on what they submitted and they’ll mention something and I’m like, “Oh, I didn’t see you put that on your form anywhere.” And they’re like, “Oh, I didn’t think it was important” or “I didn’t remember” or “I forgot.” You know, so really spending this time connecting and working through this as a team is so important because it helps to have these revelations that you wouldn’t otherwise have.
What is a Hot Mess Gut?
[00:11:33] And so you have to ask why you have to look for the themes that started off, and then you also have to look for the things that are allowing these hot mess gut symptoms to continue. Now, when I say hot mess gut. I’ll define it for you here. I actually have a whole episode where we go through what that looks like, but if you have a hot mess gut you probably already know you don’t even need me to define it.
[00:11:58] You know what it is, right? Whether you have IBD, IBS or undiagnosed gut symptoms, you know if you have a hot mess gut, if you’re missing out on life because of your digestive symptoms, you’re afraid of not being able to make it to the bathroom. You’re afraid of what to eat at restaurants, because you don’t know what’s gonna trigger your symptoms, or you do know what’s gonna trigger your symptoms and you don’t have control over what they’re putting in your dishes.
[00:12:22] If you’re afraid to travel, if you’re laying on your couch after work, you know, exhausted and in pain and barely able to make it through the day. If you’re turning down promotions at work, because you don’t think you feel well enough to be able to take on more responsibility. Like these are all ways that your gut can be impacting your life that I hear about all the time.
[00:12:46] You’re not alone. Other ways are just not being your most joyful self, not being as patient with your kids as you want to be, because you don’t feel good. Not being hungry. Losing your joy of food. You don’t enjoy your food anymore because it’s just become this thing you have to do. And you know, it’s gonna cause pain.
[00:13:05] Those are all symptoms of a hot mess gut. And then we’re gonna do another episode on this later, but your gut health impacts everything else in your body. So even if your digestive symptoms, aren’t that big of a deal, if you have autoimmune conditions, if you, you know, said, so we’re gonna go into that a little bit.
[00:13:23] So like thyroid, psoriasis, arthritis, you know, rheumatoid arthritis, lupus, those kinds of things. Those can be drawn back into the gut too. If you have histamine issues, mass cell activation issues, those can all be related to the gut as well. We’ll do a deeper dive on those. In another episode, I wanna bring us back into this hot mess gut space, but any of those I would include in this hot mess gut sphere.
[00:13:52] So, again, if you have it, you know it, right? You know it, especially after I ran through some of those examples of it, even if you’re not necessarily having a ton of digestive symptoms, if you’re having other health issues that are chronic inflammatory in nature, it’s probably linked back to your gut health.
[00:14:11] Okay? And it would benefit you to explore restoring full function to your digestive system. So we spent some time digging. We ask why we look for the things, allowing it to continue. And this is where I wanna give you guys some tips. Okay. So I wanted to share, you know, the top three things that I see contributing to people’s hot mess guts because of our culture.
Top Three Things Contributing to Your Hot Mess Gut
Stress
[00:14:40] Because of our society, because of the way we’ve grown up in our environment that you can do on your own to, to see an improvement in your digestive symptoms. So we’re gonna start with junk stress first. Okay. Junk stress is huge. And I hear all the time, people almost carrying their stress around like a badge of honor, you know?
[00:15:04] “Oh yeah. I’m so stressed out.” “Oh, me too.” You know, I get it, you know, “Oh, I’m running from this to that, to this.” And I found a lot of the time this stress or over commitment comes from lack of clarity on who we are and our priorities. And so really setting some time to be intentional with what do you value and what are your priorities.
[00:15:31] As a family, as a couple, as a person, name out a few, and then if something isn’t in line with those priorities, you can easily say no to it. And the reason is that it doesn’t align with your priorities right now. You know, you can say no. Relational stress conflict. That’s not being repaired or worked through all of those things can add to this just chronic stress.
[00:15:58] You know, that’s just weighing us down and there is a direct. Physical connection between our brains and our guts. And it’s called the vagus nerve. I love the vagus nerve. We’re gonna do another episode on vagus nerve too. But it’s this nerve that goes down to our heart, to our lungs, through our digestive tract.
[00:16:20] And it has these little fingers that insert itself all throughout and it’s so our brains and our guts connect and communicate. And for every one message that our brain sends down to our gut, our gut actually sends six messages up to our brain. So they’re very much in communication. Who’s driving the ship, right?
[00:16:40] Is it the, is it the brain or is it the gut ? We can go into that more too. But it it’s really important and our stress level very much impacts gut motility. So how fast things are moving through our gut? Slow how well we’re able to break things down and use those nutrients. Huge, huge impact. So really taking a close look at your stress, saying what you can say no to with ease, how you can minimize your stress.
[00:17:14] Do some good things that you enjoy to balance that stress going on a walk in nature can feel really calming taking some deep breaths throughout the day, focusing on joy and things to be grateful for. Those are three things that you can do right now. Plus focusing on your priorities. There’s one – giving you four tips.
[00:17:34] Go take action on one of them. Okay for reducing that junk stress, that’s just keeping you tightly wound sometimes without even realizing it, sometimes the stress can creep in and become such an integrated part of our identity. We don’t even realize that it’s not an original part of who we are and it’s the stress that we’ve just been carrying on and, and holding onto for.
Sleep
[00:17:56] So, So that stress is a big one. Junk sleep is a second one. We have to have sleep. We have to have that rest and repair overnight to really reset our bodies. You know, if you’re eating right before bed, your body is focusing on digesting that food instead of repairing parts that need to be repaired. So junk sleep and, and we’re gonna do a big episode on sleep and digestive health as well.
[00:18:27] Sleep can really impact digestion in a negative way too. So making sure that you’re doing what you can to prioritize, sleep and rest is important. And then the third one that we’re gonna go into is, as you guess, since I am a dietician is junk diet. And we’re talking about this in two different ways.
Diet
[00:18:46] We’re talking about what we eat. Yes. We’re also talking about how we eat. It’s just as important as what we’re eating. So what we’re eating, we know as Americans, we are, you know, relying on refined, packaged foods a lot of the time. And it’s because we’re, over committing ourselves a lot of the time and we’re running from one thing to the next and we’re not prioritizing, you know, making our meals at home anymore.
[00:19:13] And that is what it is sometimes, but there are some things we can do about it sometimes too, and actions we can take, whether it looks like meal planning and being more intentional about planning out meals on those busier days, doing things as a family, helping share the burden instead of putting it all on yourself, there are ways to do it, and, and live a busy lifestyle as.
[00:19:34] Prioritizing vegetables, fiber, not just those starchy carbs, you know, and the quality as well. You know, the quality of what you eat, not just getting in your vegetables, but you know, is it, is it organic? Is it covered in pesticides? Is it, you know, how is it prepared if it’s a meat product?
[00:19:54] How is that animal raised that then you’re consuming? So really taking a closer look at what we eat. And we, I go into this a lot deeper with my clients and I, you know, I get asked a lot of the time about elimination diets. I mentioned the low FODMAP diet before, and I’m gonna talk to elimination diets here for a minute.
[00:20:17] A lot of the time they are talked about to heal your gut. So reduce, you know, cut out your food sensitivities to get rid of your digestive symptoms. Go on this low FODMAP diet, go on a carnivore diet, go on a keto diet to heal your gut. The problem that I have with these, there’s a couple – there’s probably more than one I’m gonna say right here – but first of all, most of the time, if you’re having chronic digestive symptoms, you already have a damaged relationship with food.
[00:20:46] You’re already fearful of food. You’re already limiting food. It’s already kind of like, you know, not great. And I find that these elimination diets can only make that, and a lot of the time they, you know, can just really exacerbate that damaged relationship with food. They can be useful in reducing symptoms temporarily.
[00:21:10] I have a client right now, actually, where we’re talking about doing a form of an elimination diet short term to rule something out that we don’t have a good test for. So being used in a way like that can be really, really helpful, but just going on an elimination diet to heal your gut…
[00:21:30] It’s not gonna heal your gut. It’ll help you reduce your symptoms in the short term, but you need to do other things as well to actually see an improvement in your gut. Then we’re gonna go into how we eat. So oftentimes going back to that stress piece where we’re rushed, we’re not chewing our food, we’re eating on the move.
[00:21:51] We’re multitasking. And we’re not setting up up our body to really. Take this food and turn it into nutrients and digest it and absorb those nutrients and then eliminate what’s not needed. It’s really important to be in this rested, relaxed state whenever we’re eating. So if at all possible, I’m going to give you a few tips here, because these are really easy to implement as well.
How to Eat for Gut Health
[00:22:16] If at all possible before you sit down to eat, be rested and relaxed and joyful and not stressed or rushing. Sit down. At the table, not in front of the TV, not in front of distractions. Not trying to work if at all possible, take a couple of deep breaths where you’re breathing in, you’re feeling your belly expand.
[00:22:39] You’re holding it for a couple of counts and then your exhaling and your exhale is actually gonna be longer than your inhale here. And that’s gonna help you get into this relaxed state and tell your body, “Hey, we’re eating here. All as well. We’re not about to run away from a saber-toothed tiger.” We can be in this rest and digestive state, and then you’re gonna take a bite and you’re gonna chew it 30 to 40 times each bite.
[00:23:03] It needs to feel like mush whenever you swallow it. Okay? Chew 30 to 40 times. And if it feels like it’s been a crazy long time that you’ve been chewing your food, that’s a really good indication that you aren’t normally chewing your food for that. Okay, so do that. And you know, try it. I’m gonna give you this other tip too.
[00:23:24] If it feels like a long time, try it for one meal a day and then work your way up from there. Or try it for the first five bites of each meal, whichever way makes more sense from there and try to expand from there. Okay, but really chew your food well. It’s taking the burden off of your digestive system.
[00:23:41] If you’re chewing your food first, it’s gonna be a lot easier for your stomach and digestive enzymes to break that food down. If it’s already been mechanically broken down by chewing, and you also have digestive enzymes in your saliva, that helps to digest and break down that food as well. Um, so be really relaxed, take a deep breath and chew your food really, really well….
[00:24:05] …whenever you’re eating to boost your digestion and see if that helps. I have had so many people come to me and tell me that by just doing those things, they’ve seen a dramatic, like 80%, reduction in gut symptoms. That’s the goal that I use when I’m working with my clients. I always tell them, I want you to see an 80 to 90% reduction in your gut symptoms.
Recapping My Top Tips for Better Gut Health
[00:24:27] That’s my goal for you whenever we’re working together. So if somebody can do that just by changing the way that they’re eating, that’s incredible. So give that a try, see if it helps. I bet it does. So those are the three things that we’re gonna do first. You’re gonna look at your stress. See where you’re carrying stress, see where you can let go of stress, look at your sleep, and then look at what you’re eating and how you’re eating it.
[00:24:52] And see what improvements you can make. If you’ve done that you say, you know, “Katie, what if I do these things and I’m the same, it doesn’t help. Then what do I do then?” It may be some time to get some help from somebody who is going to come alongside you. Roll up their sleeves, ask the hard questions, ask the really good questions and work through it.
[00:25:14] And look for some answers. Chances are, if you have been dealing with these digestive symptoms for a long time, and you’ve tried other things you may need more than these simple tips I gave you here, there’s a good chance they will help some, but they may not get you all the way to the finish line.
[00:25:31] And that’s where you really need a personalized plan looking at what is going on in your body. That’s allowing these symptoms to continue and, then you know where to go from there. And so that’s what I’m able to do is I’m able to really make a personalized plan with my clients. We do some testing, get a better idea of what’s going on, ask really good questions.
[00:25:52] And then we’re looking at all of the things I mentioned: Stress, Sleep, Food ways to boost digestion, we’re even expanding into environmental toxins. So what you’re putting on your skin, what you’re breathing in, quality of your water, quality of your cookware, all of that, and then exercise and movement as well.
[00:26:11] So it’s, it’s really comprehensive and it goes a lot deeper, whenever you’re pairing with somebody, but I gave you some really great tips to get started today. So let me know, send me a message on Instagram, reach out, let me know which tip you’re taking action on and how it helps. If you are doing these things already and you need help,
[00:26:33] Go apply to work with me. I can help you with, I can help you come up with a personalized plan. It’s what I do all day, every day. And so we will talk soon and I hope that you guys have an awesome day.
[00:26:45] Thank you so much for listening to the entire episode. I hope you are feeling inspired and empowered to take bold action towards your health goals. If you enjoy what you heard, don’t forget to follow my show so you never miss a new episode. And it would mean the world to me, if you left me a review, so others know what to expect from my show.
[00:27:11] Last, get in touch. Let me know what bold action you’re taking. Let me know how you’re inspired. Follow me on Instagram @the_healthygut_dietitian. I’ve put a link in my show notes for you, so you can simply click and follow. Come say hi, I respond to all my messages and I can’t wait to get in touch.